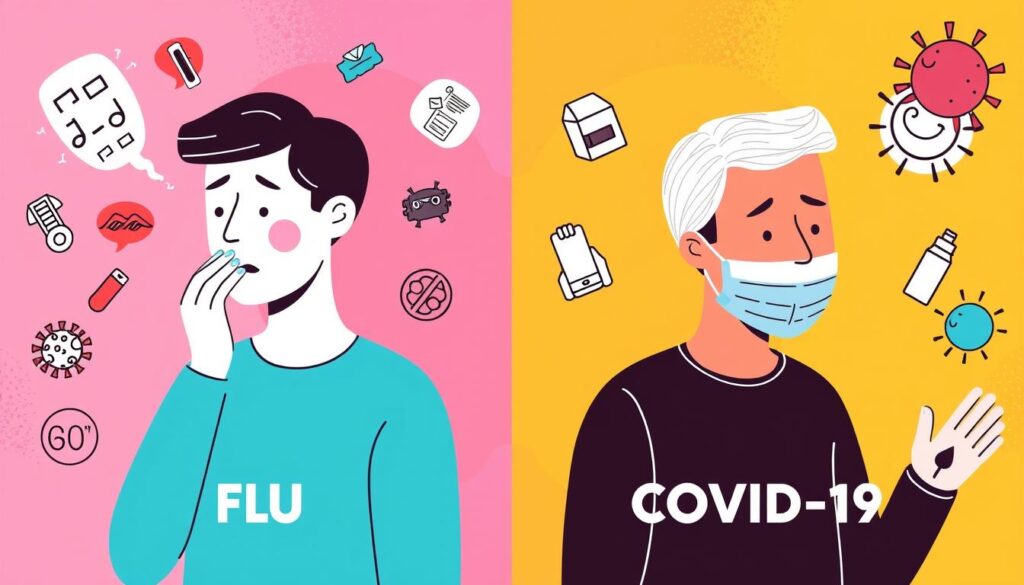
The COVID-19 pandemic has changed the world, making us all worry about the flu and coronavirus. Both are contagious illnesses, but they come from different viruses. COVID-19 is caused by SARS-CoV-2, while the flu comes from influenza A and B viruses.
Even though they share some symptoms, there are big differences. These differences are important for our health and the health of others.
One big difference is how contagious they are. COVID-19 spreads more easily than the flu. It can spread even before symptoms show up, including in people who don’t feel sick.
COVID-19 has also caused more big outbreaks than the flu. This has helped it spread fast around the world.
The severity of the illness also varies. The flu can be very bad for young kids. But COVID-19 can lead to long-term problems, like Long COVID and multisystem inflammatory syndrome. These can affect people of all ages.
Understanding the Basics: COVID-19 and Influenza
COVID-19 and the flu both harm the respiratory system. COVID-19 is caused by the SARS-CoV-2 virus. The flu is caused by influenza A and B viruses. Both can cause inflammation and damage to the airways and lungs.
But, how these viruses affect the body’s immune response is different. This difference is key to understanding their impact.
What Causes These Infections
COVID-19 was first found in late 2019. It’s caused by the SARS-CoV-2 virus. The flu, caused by influenza A and B viruses, leads to seasonal outbreaks.
Both viruses mainly attack the respiratory system. But, they can also harm other organs, causing systemic problems.
How These Viruses Impact the Body
The immune response to COVID-19 and the flu is not the same. COVID-19 can cause a severe inflammatory reaction in some. This leads to worse respiratory symptoms and a higher risk of complications.
The flu, on the other hand, has more consistent symptoms. This makes it easier to manage in many cases.
Both viral pathogens mainly hit the respiratory system. But, they affect the body in different ways. Knowing these differences is important for fighting each infection.
Transmission Methods and Infection Spread
COVID-19 and the flu spread mainly through droplets and airborne transmission. When someone with the virus coughs, sneezes, or talks, they release tiny particles. These particles can carry the virus and spread it to others through close contact or touching contaminated surfaces and then their face, mouth, or nose.
COVID-19 is often more contagious than the flu. It can lead to superspreading events where one person infects many. Also, COVID-19 might spread longer before symptoms show up.

Both viruses can spread before symptoms appear, but how and when it happens differs. Knowing how these viruses spread helps us find ways to stop them. This is key to controlling these diseases.
Flu vs Covid Symptoms: Common Signs and Manifestations
Understanding the differences between flu and COVID-19 starts with looking at common symptoms. Both fever and cough are common in both. Fatigue and muscle aches are also seen in both. But, a key difference is the loss of taste and smell, which is more common in COVID-19, affecting 38-55% of patients.
Respiratory Symptoms
Shortness of breath is often more severe and lasts longer in COVID-19 than in the flu. COVID-19 can also cause red, swollen eyes or skin rashes, like “COVID toes.”
Body-wide Symptoms
Both the flu and COVID-19 can cause headaches, sore throat, and muscle aches. But, COVID-19 symptoms usually last longer. It can also lead to more severe complications in some people.
Unique Identifying Symptoms
The loss of taste and smell is a unique sign of COVID-19, affecting many. This symptom helps doctors tell COVID-19 apart from other illnesses. It’s key for quick diagnosis and treatment.
Timeline of Symptom Development
There are key differences in when symptoms start between the flu and COVID-19. Flu symptoms show up 1-4 days after getting infected. On the other hand, COVID-19 symptoms can take 2-14 days to appear, with a longer incubation period. This means COVID-19 symptoms can start up to two weeks after exposure.
Both the flu and COVID-19 can have asymptomatic cases. This means some people might not show any symptoms. But, COVID-19 patients can stay contagious for about 8 days after symptoms start. Flu patients are usually most contagious in the first 3 days.

Knowing when symptoms start is key to telling the flu and COVID-19 apart. It helps us take the right steps to stop them from spreading. Catching and isolating sick people early can help keep communities safe.
Duration and Severity of Symptoms
The flu and COVID-19 have different symptom lengths and intensities. Flu symptoms usually go away in a few days to two weeks for mild cases. But, COVID-19 symptoms can last weeks or even months for some people. The symptom progression and recovery time depend on how severe the illness is.
Mild Cases
For milder flu cases, people usually feel better in a week. But, COVID-19 patients with mild illness might have symptoms like loss of taste and smell, fatigue, and cough for 10 days or more. About 40% of COVID-19 patients have lost their sense of smell, a rare symptom in flu patients.
Severe Cases
Severe cases of both the flu and COVID-19 may need hospitalization and can be life-threatening. COVID-19 is more likely to cause severe illness and death, mainly in older adults and those with health issues. Shortness of breath with COVID-19 can last for weeks or months, being more severe than the flu.
It’s important to watch symptoms closely and get medical help if they get worse or last too long. Rest and staying hydrated can help in recovering from both the flu and COVID-19.
Distinctive COVID-19 Indicators
COVID-19 and the flu share many symptoms. But, there are key differences. One major sign of COVID-19 is losing taste and smell, known as ageusia and anosmia. This is rare in flu cases.
These sensory issues can last for weeks or months. This is called Long COVID, affecting many body systems.
COVID-19 also causes a rare but serious condition. It’s called Multisystem Inflammatory Syndrome (MIS-C in kids and MIS-A in adults). This makes different body parts inflamed. It’s not seen in flu cases, making it a clear sign of COVID-19.

In the early days of the pandemic, symptoms like red eyes and lost taste and smell were common. Now, they’re less common in most cases. But, the lasting effects on senses and the risk of long-term problems are key differences from the flu.
Risk Factors and Vulnerable Populations
COVID-19 and influenza are more dangerous for some groups. This includes older adults, people with health issues, pregnant women, and babies. It’s key to know who’s most at risk to keep them safe.
Age-related Risks
People over 65 face a big risk from COVID-19. In the U.S., by March 2024, 76% of COVID-19 deaths were in this age group. Babies under 6 months also have a high risk of serious illness from COVID-19.
Medical Conditions
Those with lung diseases, heart issues, diabetes, or weak immune systems are at higher risk. Lung damage from conditions like asthma or COPD can lead to serious COVID-19 complications. Cancer patients, Down syndrome, ADHD, or cerebral palsy individuals also have a higher risk.
The FDA has approved pemivibart (Pemgarda) for immunocompromised individuals. It helps those who may not get full protection from vaccines. It’s important for those at risk to wear masks, stay far apart, and follow good hygiene to avoid these viruses.

Potential Complications and Long-term Effects
COVID-19 and influenza can both cause serious problems. But, research shows COVID-19 might be more dangerous. Both viruses can lead to pneumonia and other severe conditions. Yet, COVID-19 is linked to more life-threatening blood clots in different organs.
Long COVID is a condition some people face after getting COVID-19. It can cause symptoms to last for months. These symptoms include feeling very tired, brain fog, and issues with smell and taste.
Influenza often leads to secondary bacterial infections. But COVID-19 is more likely to cause inflammatory conditions. These can affect many parts of the body, like MIS-C and MIS-A in children and adults.
A study found COVID-19 patients were 50% more likely to die than those with seasonal flu over 18 months. They also faced a higher chance of being readmitted to the hospital and needing ICU care. The long-term effects of COVID-19 were worse, with a 68% increased risk of organ system problems, compared to just 6% for flu.
Testing and Diagnosis Methods
It’s important to tell COVID-19 apart from the flu for the right treatment. Both can be found with PCR tests and rapid antigen tests. Some tests can spot both viruses at once. But, antibody tests show if you’ve had the virus before, not if you have it now.
Getting tested early is key. PCR tests are top-notch for finding SARS-CoV-2. Antigen tests give fast results but might miss some cases. If an antigen test is negative, test again 48 hours later to be sure.
Available Test Types
Testing is key because COVID-19 and the flu share symptoms. PCR tests and rapid antigen tests can find the virus. This helps doctors give the right care and manage the disease.
When to Get Tested
Test as soon as symptoms show up or after being exposed. Early testing is key for quick treatment and stopping the virus spread. Accurate and fast testing is essential in fighting these illnesses.

Treatment Approaches and Options
Managing the flu and COVID-19 involves using antiviral medications. For the flu, drugs like oseltamivir (Tamiflu) are given within 48 hours of symptoms starting. They help shorten and lessen the illness’s severity. For COVID-19, treatments like remdesivir and Paxlovid are used in high-risk patients. They aim to prevent severe disease.
Supportive care is vital for both illnesses. This includes oxygen therapy, managing fluids, and treating complications. In severe cases, hospitalization may be needed. This is true for those with underlying health issues or at high risk of complications.
Early treatment is critical for both the flu and COVID-19. It can lower the risk of severe illness and hospitalization. By knowing the treatment options and seeking medical help quickly, people can manage their symptoms. This helps lessen the impact of these viral infections.

Prevention Strategies and Vaccines
Keeping yourself and your loved ones safe from the flu and COVID-19 is key. Vaccines are out for both viruses. It’s important to keep your vaccinations current. You should get a flu shot every year. For COVID-19, you need initial doses and boosters to stay protected.
Preventive steps for both viruses include social distancing, mask-wearing in risky places, and frequent hand hygiene. Staying away from crowded spots and washing your hands often can lower infection risks.
The FDA has okayed new mRNA COVID-19 vaccines for 2024. The CDC also suggests getting the updated flu vaccine by October for the 2024-2025 season. This will help protect against three types of the flu virus. By being proactive and following these steps, you can keep yourself and your community safe.
When to Seek Medical Attention
Most cases of COVID-19 and flu can be treated at home. But, knowing when to seek medical help is key. Look for emergency signs like trouble breathing, chest pain, confusion, or trouble staying awake. These signs mean you need help fast to avoid serious problems.
Emergency Warning Signs
Don’t wait if you see symptoms like trouble breathing or chest pain. Also, watch for sudden confusion, trouble staying awake, or blue lips. These signs mean you need emergency care right away.
High-risk Situations
Some people are more at risk, like older adults, pregnant women, and those with health issues. If you think you have an infection, call your doctor fast. Early care is important to keep you safe, even more so for these groups.